Endocrine Journal Club
Dr. Mundi, Dr. Laidlaw, and Dr. Lee would like to welcome you the Endocrine Journal Club.
Monday, May 12, 2014
health places
Friday, April 18, 2014
Perspectives of Physicians and Nurse Practitioners on Primary Care Practice
Background
The U.S. health care system is at a critical juncture in health care workforce planning. The nation has a shortage of primary care physicians. Policy analysts have proposed expanding the supply and scope of practice of nurse practitioners to address increased demand for primary care providers. These proposals are controversial.
http://www.nejm.org/doi/full/10.1056/NEJMsa1212938?query=TOC#t=abstract
Wednesday, March 26, 2014
Wednesday, February 19, 2014
Insulin: Potential Negative Consequences of Early Routine Use in Patients With Type 2 Diabetes
http://care.diabetesjournals.org/content/34/Supplement_2/S225.full
--
Assistant Professor of Clinical Medicine
“This email message is confidential, intended only for the recipient(s) named above and
may contain information this is privileged, exempt from disclosure under applicable law.
If you are not the intended recipient, do not disclose or disseminate this message to
anyone except the intended recipient. If you have received this message in error, or are
not the named recipient(s), please immediately notify the sender by return email, and
delete all copies of this message.”
Tuesday, February 18, 2014
tweet embed
A Mariachi musician stands along Cesar Chavez Blvd in Boyle Heights.
#mariachi #bass #music #boyleheights #losangeles pic.twitter.com/6mHwYSEjoO
— luis sinco (@luissinco) February 13, 2014Wednesday, January 15, 2014
"Abdandon LDL targets? Not yet" Commentary
Commentary Link
Also this regarding the AACE postion
Thursday, December 19, 2013
Counterpoint from ORIGIN Hypoglycemia Subanalysis
- When patients with dysglycemia had severe hypoglycemia while on treatment with basal insulin glargine, the episodes did not trigger as many adverse cardiovascular outcomes as did severe hypoglycemia during standard care with oral glucose-lowering drugs but no insulin.
- "Hypoglycemia caused by insulin glargine–mediated glucose lowering is unlikely to cause cardiovascular outcomes," Dr. Linda G. Mellbin said at the European Society of Cardiology Congress 2013.
- "What was reassuring was that while insulin glargine caused more hypoglycemic events" compared with standard treatment in these patients, "the absolute number of fatal events was still lower with insulin, showing insulin is a very safe treatment," said Dr. Lars Rydén, professor of cardiology at the Karolinska Institute and a coinvestigator with Dr. Mellbin.
- This study highlights the clear relationship between severe hypoglycemias with death and cardiovascular mortality. There are more severe hypoglycemias with lantus than standard oral therapy. [This highlights the clear added risk when you introduce lantus for therapy.] There is a 3 fold risk of inducing symptoms so severe that you need assistance.
- People had been supporting glargine through claiming that it is a smooth, peakless insulin. In this study, it shows that glargine is not better than stardard of care sulfonureas. It does not provide any cardiovascular advantage nor is it safer than sulfonureas.
- We know from the UKPDS that early aggressive control can provide cardiovascular benefit. We know from previous subanalysis of the ORIGIN trial, that patients on glargine had better durable glycemic control. Another substudy from Diabetes Care show that the IMT carotids were a bit better in the glargine group. The question that needs to be asked is: "Is hypoglycemia is so bad with the lantus group that it is negating the positive benefit of glycemic control."
- How can you draw conclusions about nocturnal hypoglycemia. The absolute numbers between the lantus and control is 100 vs 18. 18!!
- If you treat your stable diabetics with lantus and titrate them to 95, you will get a high report of nonsevere and severe hypoglycemia, which obliterates any metabolic benefit you achieve using this regimen. You will also expect weight gain of 1.6kg of weight gain and more reports of new angina pectoris.
Points: Origin Hypoglycemia Subanalysis
1. 12,537 patients with known CV disease recruited into prospective study from 573 centers from around the world. Randomized to standard care vs glargine. With glargine titrated to fasting glucose <=95 by self-measurement. Study powered to detect 18% and 16% relative risk reduction in primary outcome and secondary outcome. All patients self-monitored and logged glucose levels. Median follow up 6.2 yrs. 99% outcome status known. Primary outcome: composite non-fatal MI, non-fatal CVA, or death from CV cause. Secondary outcome: any of primary events, a revascularization procedure, or hospitalization for heart failure. Points in favor of the Origin study are the power of study, prospective, randomized and using patients who had known CV disease and therefore at higher risk for an event. The subanalysis included all patients and data from the original study.
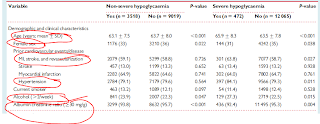
2. From table 2: Significant elevated hazard score in severe hypoglycemia for each endpoint shown: CV death or non-fatal MI or stroke 1.77, Total mortality 2.05, CV death 2.02, Arrhythmic death 2.14. Unadjusted hazard for severe nocturnal hypoglycemia was also significantly elevated in all 4 categories. The unadjusted hazard for non-severe mortality was also significantly elevated at 1.21.
3. From table 3: Incidence of hypoglycemia both non-severe and severe is higher in insulin glargine group versus standard care.
4. Although the crude incidence of mortality, cv death, arrhythmic death, and CV death-non-fatal MI-CVA in both severe and non-severe hypoglycemia is higher in the glargine group than the standard group, overall there was no difference in mortality or cv events between the two groups if one includes both hypoglycemia and absence of hypoglycemia.
5. The findings of an association between severe hypoglycemia and CV outcomes is consistent with prior studies showing a similar association.
Monday, December 16, 2013
Does hypoglycaemia increase the risk of cardiovascular events? A report from the ORIGIN trial
Does hypoglycaemia increase the risk of cardiovascular events? A report from the ORIGIN trial
Abstract
Point Counterpoint
Idea:
Find a study which is relevant to clinical practice and has a new/unexpected outcome.
One expert takes the "point" position the other takes the "counterpoint" position.
Each expert independently dissects the paper and comes up with 5 points. One will have five points in favor of supporting why we should believe the outcome. The other will have 5 points showing why the outcome is probably not valid.
Essentially what we're trying to find out is should our practice change in some way based on the findings?
We will do 3 papers per month and alternate the point counterpoint positions.
The first will be Dr. Lee and Dr. Laidlaw with the paper "Does hypoglycaemia increase the risk of cardiovascular events? A report from the ORIGIN trial".
The program will work as follows:
1. 3 papers chosen per month
2. The person choosing the paper for that week will be "point". (The person choosing the next week's paper will be counterpoint).
3. Upload the paper to Zotero and notify via the blog (title of paper and abstract ideally).
4. On Thu each expert will separately post their 5 points and counterpoints.
5. Then anyone can chime in with comments and potentially come to some consensus thought on the matter.
Let the games begin!
Friday, August 9, 2013
The BRAF V600E mutation in papillary thyroid cancer with positive or suspected pre-surgical cytological finding is not associated with advanced stages or worse prognosis.
- lookahead, nejm, lifestyle
- shah, jcem, dppiv
- sung, jcem, fatty liver
- chowdhury, journal of physio pharm, MIS
- stylopolous, science, roux limb
- haddow, jcem, sigmoidal
- chen, thyroid, graves cancer
- Minakaren, cochrane db of sys review, rituximab
- itterman, clinical thyroid, Metformin
- Barbaro, Endocrine, BRAF
Tuesday, August 6, 2013
Metformin Prevents Goiter in Patients with Type 2 Diabetes
- lookahead group, nejm, lifestyle
- shah, jcem, dppiv
- sung, jcem, fatty liver
- chowdhury, journal of physio pharm, MIS
- stylopolous, science, roux limb
- Haddow, jcem, sigmoidal
- chen, thyroid, graves cancer
- Minakaren, cochrane Db of sys review, rituximab
- Itterman,clinical thyroid, Metformin
Sunday, August 4, 2013
Rituximab for thyroid-associated ophthalmopathy
Lookahead, NEJM, lifestyle
Shah, JCEM, dppiv
Sung, JCEM, fatty liver
Chowdhury,Can J Physio Pharm, MIS
Stylopolous, Science, Roux limb
Haddow, JCEM, sigmoidal
Chen, Thyroid, Graves cancer
Minakaran, Cochran DB Syst Rev, Rituximab
http://www.ncbi.nlm.nih.gov/pubmed/23728689
Monday, July 29, 2013
Higher cancer in graves disease
Shah,jcem,dppiv
Sung,jcem,fatty liver
Chowdhury,can j physio pharm,mis
Stylopolous,science,roux limb
Haddow, jcem, sigmoidal
Chen,thyroid,graves cancer
http://online.liebertpub.com/loi/THY#/doi/full/10.1089/thy.2012.0568
Sent from my iPhone
The relationship between TSH and free T4 in a large population is complex, non-linear and differs by age and gender
http://jcem.endojournals.org/content/early/2013/05/13/jc.2012-4223
Saturday, July 27, 2013
Reprogramming of Intestinal Glucose Metabolism and Glycemic Control in Rats After Gastric Bypass
- Stylopoulos,Science, Roux Limb
Reprogramming of Intestinal Glucose Metabolism and Glycemic Control in Rats After Gastric Bypass
- Nima Saeidi1,2,3,*,
- Luca Meoli1,*,
- Eirini Nestoridi1,*,
- Nitin K. Gupta1,
- Stephanie Kvas1,
- John Kucharczyk1,
- Ali A. Bonab2,
- Alan J. Fischman2,
- Martin L. Yarmush2,3,
- Nicholas Stylopoulos1,†
+Author Affiliations
- 1Center for Basic and Translational Obesity Research, Division of Endocrinology, Boston Children's Hospital, Harvard Medical School, Boston, MA 02115, USA.
- 2Shriners Hospital for Children, Boston, MA 02114, USA.
- 3Center for Engineering in Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA 02114, USA.
- ↵†Corresponding author. E-mail: Nicholas.Stylopoulos@childrens.harvard.edu
-
↵* These authors contributed equally to this work.
The resolution of type 2 diabetes after Roux-en-Y gastric bypass (RYGB) attests to the important role of the gastrointestinal tract in glucose homeostasis. Previous studies in RYGB-treated rats have shown that the Roux limb displays hyperplasia and hypertrophy. Here, we report that the Roux limb of RYGB-treated rats exhibits reprogramming of intestinal glucose metabolism to meet its increased bioenergetic demands; glucose transporter-1 is up-regulated, basolateral glucose uptake is enhanced, aerobic glycolysis is augmented, and glucose is directed toward metabolic pathways that support tissue growth. We show that reprogramming of intestinal glucose metabolism is triggered by the exposure of the Roux limb to undigested nutrients. We demonstrate by positron emission tomography–computed tomography scanning and biodistribution analysis using 2-deoxy-2-[18F]fluoro-D-glucose that reprogramming of intestinal glucose metabolism renders the intestine a major tissue for glucose disposal, contributing to the improvement in glycemic control after RYGB.
Thursday, July 25, 2013
Lifestyle impact on meal-induced insulin sensitization in health and prediabetes: a focus on diet, antioxidants, and exercise interventions.
Lookahead, NEJM, lifestyle
Shah, JCEM, DPP-4
Sung, JCEM , Fatty liver
Chowdhury, Can J Physio Pharm, MIS
http://www.ncbi.nlm.nih.gov/pubmed/23458192
Wednesday, July 24, 2013
Resolution of fatty liver and risk of incident diabetes
shah,jcem,dpp-4
Sung,jcem,fatty liver
http://m.jcem.endojournals.org/content/early/2013/07/18/jc.2013-1519.abstract
Sent from my iPhone
Tuesday, July 23, 2013
The DPP-4 Inhibitor Linagliptin Restores β-Cell Function and Survival in Human Isolated Islets Through GLP-1 Stabilization
http://jcem.endojournals.org/content/98/7/E1163.abstract
(lookahead, NEJM, lifestyle)
Monday, July 22, 2013
Cardiovascular Effects of Intensive Lifestyle Intervention in Type 2 Diabetes — NEJM
http://www.nejm.org/doi/full/10.1056/NEJMoa1212914#article
Sent from my iPhone
Thursday, February 14, 2013
[50] New Beta-Cell Paradigm?
Wednesday, February 13, 2013
[49] What is the impact of high triglyceride levels in severely burned pediatric patients?
#MP111212
[Kraft, JCEM, 2013, burn, triglycerides, hepatomegaly]
http://www.ncbi.nlm.nih.gov/pubmed/23150682
- Pediatric severe (30-70% BSA) burn patients stratified: normal n=127, elevated FFA 46, and elevated TG 63
- TG levels increased in all 3 groups over time
- High TG spent longest time in ICU, had highest multiorgan failure, and mortality compared to normal
- Normal and high TG required more insulin between d8 and 23
- Hepatic acute phase reactants significantly increased in TG group compared to normal
- Liver size increased in Tg group compared to normal and FFA patients
Association of postburn Fatty acids and triglycerides with clinical outcome in severely burned children.
Source
F.A.C.S., F.C.C.M., F.R.C.S.(C.),Sunnybrook Health Sciences Centre, Department of Surgery, Division of Plastic Surgery, University of Toronto, Sunnybrook Research Institute, Room D704, 2075 Bayview Avenue, Toronto, Ontario, Canada M4N 3M5. marc.jeschke@sunnybrook.ca.
Abstract
Context: Free fatty acids (FFAs) and triglycerides (TGs) are altered postburn, but whether these alterations are associated with postburn outcomes is not clear. Objective: The aim of the present study was to analyze lipid metabolic profiles in pediatric burn patients and to correlate these profiles with patient outcomes and hospital courses. Design and Setting: We conducted a prospective cohort study at an academic pediatric hospital burn center. Patients: Our study included 219 pediatric burn patients. Main Outcome Measures: Patients were stratified according to their plasma TG and FFA levels. Main patient outcomes, such as postburn morbidity and mortality, and clinical metabolic markers were analyzed. Results: All groups were similar in demographics and injury characteristics. Patients with elevated TGs had significantly worse clinical outcomes associated with increased acute-phase protein synthesis indicating augmented inflammation and hypermetabolism, whereas increased FFAs did not seem to profoundly alter postburn outcomes. Conclusions: Elevated TGs, but not FFAs, postburn are associated with worsened organ function and clinical outcomes.
Monday, February 11, 2013
[48] Is metabolic syndrome in adolescents associated with brain abnormalities?
[Yau, Pediatrics, 2012, Metabolic syndrome, executive functioning, hippocampus]
http://www.ncbi.nlm.nih.gov/pubmed/22945407
Obesity and metabolic syndrome and functional and structural brain impairments in adolescence.
Source
Department of Psychiatry, New York University School of Medicine, 145 East 32nd St, 8th Floor, New York, NY 10016, USA.
Abstract
BACKGROUND:
The prevalence of metabolic syndrome (MetS) parallels the rise in childhood obesity. MetS is associated with neurocognitive impairments in adults, but this is thought to be a long-term effect of poor metabolism. It would be important to ascertain whether these brain complications are also present among adolescents with MetS, a group without clinically manifest vascular disease and relatively short duration of poor metabolism.
METHODS:
Forty-nine adolescents with and 62 without MetS, matched on age, socioeconomic status, school grade, gender, and ethnicity, received endocrine, MRI, and neuropsychological evaluations.
RESULTS:
Adolescents with MetS showed significantly lower arithmetic, spelling, attention, and mental flexibility and a trend for lower overall intelligence. They also had, in a MetS-dose-related fashion, smaller hippocampal volumes, increased brain cerebrospinal fluid, and reductions of microstructural integrity in major white matter tracts.
CONCLUSIONS:
We document lower cognitive performance and reductions in brain structural integrity among adolescents with MetS, thus suggesting that even relatively short-term impairments in metabolism, in the absence of clinically manifest vascular disease, may give rise to brain complications. In view of these alarming results, it is plausible that obesity-associated metabolic disease, short of type 2 diabetes mellitus, may be mechanistically linked to lower the academic and professional potential of adolescents. Although obesity may not be enough to stir clinicians or even parents into action, these results in adolescents strongly argue for an early and comprehensive intervention. We propose that brain function be introduced among the parameters that need to be evaluated when considering early treatment of childhood obesity.
[47] Are bisphosphonates associated with an increased risk of GI cancers?
[Vinogradova, BMJ, 2013, bisphosphonates, GI cancer, adjusted odds ratio]
http://www.ncbi.nlm.nih.gov/pubmed/23325866
BMJ. 2013 Jan 16;346:f114. doi: 10.1136/bmj.f114.
Exposure to bisphosphonates and risk of gastrointestinal cancers: series
of nested case-control studies with QResearch and CPRD data.
Vinogradova Y, Coupland C, Hippisley-Cox J.
Source
Division of Primary Care, University Park, Nottingham NG2 7RD, UK.
Abstract
OBJECTIVE:
To investigate the association between use of bisphosphonates estimated
from prescription information and risk of gastrointestinal cancers.
DESIGN:
Series of nested case-control studies.
SETTING:
General practices in the United Kingdom contributing to the QResearch
primary care database (660) and the Clinical Practice Research Datalink
(CPRD) (643).
PARTICIPANTS:
Patients aged ≥50 with a diagnosis of a primary gastrointestinal cancer
in 1997-2011, each matched with up to five controls by age, sex,
practice, and calendar year.
MAIN OUTCOME MEASURES:
Odds ratios for incident gastrointestinal cancers (colorectal,
oesophageal, gastric) and use of bisphosphonates, adjusted for smoking
status, ethnicity, comorbidities, and use of other drugs.
RESULTS:
20 106 and 19 035 cases of colorectal cancer cases, 5364 and 5135 cases
of oesophageal cancer cases, and 3155 and 3157 cases of gastric cancer
were identified from QResearch and CPRD, respectively. Overall
bisphosphonate use (at least one prescription) was not associated with
risk of colorectal, oesophageal, or gastric cancers in either database.
Adjusted odds ratios (95% confidence interval) for QResearch and CPRD
were 0.97 (0.79 to 1.18) and 1.18 (0.97 to 1.43) for oesophageal cancer;
1.12 (0.87 to 1.44) and 0.79 (0.62 to 1.01) for gastric cancer; and 1.03
(0.94 to 1.14) and 1.10 (1.00 to 1.22) for colorectal cancer. Additional
analyses showed no difference between types of bisphosphonate for risk
of oesophageal and colorectal cancers. For gastric cancer, alendronate
use was associated with an increased risk (1.47, 1.11 to 1.95; P=0.008),
but only in data from the QResearch database and without any association
with duration and with no definitive confirmation from sensitivity analysis.
CONCLUSIONS:
In this series of population based case-control studies in two large
primary care databases, exposure to bisphosphonates was not associated
with an increased risk of common gastrointestinal cancers.
PMID: 23325866 [PubMed - in process] PMCID: PMC3546625 Free PMC Article
Thursday, February 7, 2013
[46] Are androgen levels elevated in postnatal infant acne and sebaceous gland hypertrophy?
[Kuiri-Hanninen, JCEM, 2013, Acne, testosterone, 46]
http://www.ncbi.nlm.nih.gov/pubmed/23144469
Transient postnatal secretion of androgen hormones is associated with acne and sebaceous gland hypertrophy in early infancy.
Source
University of Eastern Finland and Kuopio University Hospital, P.O. Box 1777, FI-70211 Kuopio, Finland. ulla.sankilampi@kuh.fi.
Abstract
Context: Sebaceous gland hypertrophy (SGH) and acne-like skin eruptions are frequent during the first months of life, yet the etiology and prevalence of these conditions in infants are not clear. Objective: The objective of the study was to evaluate the association of postnatal androgens with SGH and acne in infants. Design: This was a longitudinal, monthly follow-up from 1 wk (D7) to 6 months of age (M1-M6). Patients: Patients included 54 full-term (FT; 26 boys) and 48 preterm (PT; gestational age at birth 27.7-36.6 wk, 22 boys) infants. Main Outcome Measures: The occurrence of SGH (present/absent) and acne (5-10, 10-50, and >50 papules) was registered and compared with urinary levels of dehydroepiandrosterone and its sulphate and testosterone measured by liquid chromatography-tandem mass spectrometry. Results: SGH was observed in 89% of FT and 96% of PT infants (P = 0.28). Acne (more than five papules) was observed in 91% of FT infants and in 75% of PT infants (P = 0.06). Both SGH and acne were associated with developmental rather than calendar age: SGH was limited to postmenstrual age less than 46 wk and acne was not observed less than 37 wk of postmenstrual age. Urinary androgen levels showed severalfold differences in magnitude between sexes and between the FT and PT groups. After grouping according to sex and maturity, the occurrence of SGH and the severity of acne were associated with higher urinary dehydroepiandrosterone sulphate and testosterone levels in each group. Conclusions: SGH and acne are common during the first months of life and associated with endogenous, physiologically elevated levels of androgens originating from the adrenals and gonads. These data suggest a novel role for postnatal androgen secretion in infancy.
Wednesday, January 30, 2013
Deer Antlers
Monday, January 14, 2013
MP 41-45
[45] spit as good as urine for cylic cushing's
A Comparison of the Use of Urinary Cortisol to Creatinine Ratios and Nocturnal Salivary Cortisol in the Evaluation of Cyclicity in Patients with Cushing's Syndrome
- Author Affiliations
- Regional Centre for Endocrinology and Diabetes (U.M.G., S.J.H., K.R.M., A.B.A.) and Regional Endocrine Laboratory (M.McD.), Royal Victoria Hospital, Belfast BT12 6BA, United Kingdom
- Address all correspondence and requests for reprints to: Dr. Una Graham, Regional Centre for Endocrinology and Diabetes, Royal Victoria Hospital, Grosvenor Road, Belfast BT12 6BA, United Kingdom. E-mail: qublbc8@hotmail.com.
Abstract
Context: Cyclical Cushing's syndrome is detected in our center by collecting sequential early morning urine (EMU) samples for cortisol to creatinine ratio over 28 d. The Endocrine Society suggests that nocturnal salivary cortisol (NSC) may be used to assess patients for cyclical Cushing's. However, there is only very limited evidence that it correlates with EMU testing or that it demonstrates cycling over 28 d.
Objective: We sought to correlate NSC with EMU results collected the following morning and to determine whether NSC could be used to detect cyclical Cushing's.
Design and Setting: An observation study of 28-d collections for NSC and EMU was performed in a tertiary referral center over 1 yr.
Patients: A 28-d collection of NSC and EMU was performed in 10 patients with confirmed or suspected Cushing's syndrome.
Main Outcome Measure: The main outcome of the study was the correlation of salivary and urinary cortisol with graphical assessment of results for cycling.
Results: Eleven collections were performed. One patient with cyclical Cushing's completed the collection before and after cabergoline therapy. Two hundred seventy matched salivary and urinary results were correlated (r = 0.79; P < 0.001). In two patients with cyclical Cushing's, EMU and NSC followed a similar cyclical pattern. In one patient with recurrent cyclical Cushing's, cortisol was elevated in both saliva and urine but with more prominent cycles in saliva.
Conclusion: NSC correlated well with EMU. NSC detected all cases of cyclical Cushing's. Therefore, NSC may prove to be an additional option or replacement for EMU in detecting cyclical Cushing's syndrome.